Case Conceptualization
Brief Summary
Marci, a 22-year-old female college student, is undergoing therapy after being arrested for driving while impaired (DWI) five months prior. She had a 0.13 alcohol level and was also found to be in possession of about 1 gram of marijuana. Although she has a suspended license due to this incident, she has been granted permission to drive to work and school. Marci has a history with several substances: nicotine, marijuana, and alcohol. She started smoking cigarettes when she was 16 and currently smokes one pack per day. She began testing out marijuana when she was 17 and has been smoking two to three times a week for the past year. Alcohol was introduced when she was 13 by her parents by drinking wine with dinner and became a “serious” drinker around the age of 18. For the past year she has been drinking four or more alcoholic drinks three to four times a week, with an emphasis placed on drinking and smoking on the weekend with friends. However, the past two months she has been drinking one to two glasses of wine and half a joint of marijuana on her own on weeknights. Since her arrest, she has mostly been using alcohol rather than marijuana. Two months ago, she also started feeling sadness, excessive worry, and “depressed and anxious”, but has not had suicidal ideation or panic attacks. She is also worried that her period is late. Most important issues to tackle include her substance abuse, possible depression, and physical health.
Past and Current Substances Used and their Effects
Nicotine
Nicotine is normally inhaled through smoking but can also be absorbed through mucous membranes. Physiological and behavioral effects of addiction to nicotine include shortness of breath during exertion, increased heart rate and blood pressure, mild stimulant effects, and withdrawal symptoms when not allowed to smoke (Hart & Ksir, 2018). The process of addiction is similar to the process involved in addiction to heroin or cocaine (Hart & Ksir, 2018). Smoking has been repeatedly linked specifically with lung cancer, but also with all other types of cancer (Hart & Ksir, 2018). It has also been associated with cardiovascular disease and chronic obstructive lung disease (Hart & Ksir, 2018). Harmful side effects are also present for infants born to smoking mothers. The strongest link reported between smoking and pregnancy is a lower birth weight for infants which may be tied to deficiencies in their growth rate and cognitive development (Hart & Ksir, 2018).
Cannabis
Cannabis can be used through smoking the actual plant bud, using vape pens for extracts, or ingesting edibles (Hart & Ksir, 2018). General addictive effects of cannabis include “ratings of euphoria, high, mellowness, hunger, and stimulation after smoking marijuana” (Hart & Ksir, 2018, p.342). Harmful side effects are possible for people with impaired cardiovascular systems due to increased heart rate (Hart & Ksir, 2018). For long-time, heavy smokers a risk of reduced pulmonary function is present (Hart & Ksir, 2018). Smokers may also experience symptoms of chronic bronchitis – including cough and phlegm, increased anxiety while using, a reduction in immune system functioning, and significant impairments in the ability to operate machinery (Hart & Ksir, 2018).
Alcohol
Alcohol is consumed as a beverage. The most common forms of the beverage are beer, wine, and distilled spirits. General addictive effects include a reduction of inhibitions, increased behavioral activity, euphoria, and disruption of critical thinking leading to reduction in anxiety (Hart & Ksir, 2018). Harmful side effects include impaired reaction time, slower blood clotting, affect of every neurotransmitter in the brain, and alcohol poisoning (Hart & Ksir, 2018). Chronic users are at risk of having every organ system affected, including brain damage, liver disorders, heart disease, and cancer (Hart & Ksir, 2018).
Risk/Dangers for Client
There are several possible dangers for Marci. First, her consumption of a pack of cigarettes a day is considerably putting her health at risk, already experiencing a dry cough. Because she is not wanting to quit any of the drugs she uses, she is also still at risk of accidents of driving while impaired. Additionally, her mental health is suffering as she feels bad about herself, putting her at risk of developing other addictions to prescription pills she has been offered. Her lack of knowledge about being possibly pregnant indicates risk related to involvement in being sexually active. Her spiritual state is also in danger of apostasy as she abandons the faith her parents brought her up in. Risk management would include collaborating with the client on goals to remove possible dangerous situations. However, this needs to be addressed carefully since she is a pre-contemplation stage of change. She may feel defensive about efforts to help her quit, therefore collaboration on goals for safety would be more effective at reducing defensiveness (The Stages of Change, n.d.). Risk management would also include an explanation and personalization of the risks she is participating in (The Stages of Change, n.d.).
AUDIT Scores and Explanations
Item 1 in the AUDIT refers to how often a drink containing alcohol is consumed. Based on Marci’s narrative stating she drank 3-4 times a week, I selected 4 or more times a week. Although I was not sure if I should select the lower range of 2-3 present, I went ahead with 4 or more. This gave her a score of 4 on this question.
Item 2 in the AUDIT refers to how many drinks containing alcohol are consumed in a day there has been drinking. Marci stated that she typically will drink 4 or more drinks on the day she chooses to drink. I selected answer 3 or 4, although this may be underrepresenting her actual number, it would balance out the chosen answer for the previous question. This gave her a score of 1 on this question.
Item 3 in the AUDIT refers to how often six of more drinks are consumed on one occasion. Marci stated that on Saturday evenings she often drinks six to seven beers at parties. Therefore, this type of drinking was occurring weekly. This gave her a score of 3 on this question.
Item 4 in the AUDIT asks how often during the last year she has found that she was not able to stop drinking once she started. Due to lack of information in the narrative, I chose never. Also, Marci does not seem to think that her drinking is a problem, therefore I assumed that she has not really tried to cut down or stop drinking. One exception to this is the mention that when her parents pressed her about her drinking and smoking marijuana, she abstained for a couple of weeks. This gave her a score of 0 on this question.
Item 5 in the AUDIT pertains to how often during the last year she has failed to do what was normally expected of her because of her drinking. Marci stated that the mornings after using alcohol she would tend to skip class in the mornings, but not every week. She also has not been able to follow the law and drive sober several times. Based on this I selected monthly as the answer to this question, which gave her a score of 2 on this question.
Item 6 in the AUDIT refers to how often a drink is needed in the morning to get going after a heavy drinking session. Marci stated that the next day after she goes to parties, she begins to drink at lunchtime but did not state specifically needing a drink to get going. Therefore, it seemed appropriate to select never. This gave her a score of 0 on this question.
Item 7 in the AUDIT asks how often guilt or remorse is felt after drinking. Although Marci did not express concerns about her use of alcohol, she did express guilt over the way it was affecting her relationship with her parents and her educational goals since her arrest. Therefore, I selected less than monthly, since it seems only specific situations bring about these feelings. This gave her a score of 1 on this question.
Item 8 in the AUDIT refers to how often during the last year she has not been able to remember what happened the night before because she had been drinking. There was nothing in the narrative that pointed to this being a problem for her therefore I selected never. This gave her a score of 0 on this question.
Item 9 in the AUDIT asks if the person themselves or anyone else has been injured as a result of the drinking. Although in her minor accidents she has not injured others, she was injured herself therefore I selected yes, during the last year. This gave her a score of 4 on this question.
Item 10 in the AUDIT asks if a relative, friend, doctor, or health care worker has been concerned about the drinking or suggested she cut down. It is clear from the narrative her parents have asked her. Additionally, she has been referred to counseling for the issues related to her use. Therefore, I selected yes, during the past year. This gave her a score of 4 on this question.
The answers selected give Marci a total score of 19. This score indicates hazardous and harmful alcohol use. Possibly, alcohol dependence is also an issue. Also, the last two questions indicate alcohol related harm is already being experienced. Therefore, this score represents a high level of risks related to alcohol and high level of alcohol problems.
Referrals/Resources/Recommendations
AUDIT scores recommend managing with “simple advice, brief counseling and continued monitoring” by falling in a Zone III risk level (World Health Organization, 2001, p.21). Brief interventions recommended by the World Health Organization (WHO) in the AUDIT include (World Health Organization, 2001, p.22):
- “Present screening results
- Identify risks and discuss consequences
- Provide medical advice
- Solicit patient commitment
- Identify goal – reduced drinking or abstinence
- Give advice and encouragement”
Additionally, the following recommendations are suggested to motivate the client to abstain from drinking and smoking as a form of self-medication.
- Motivational Interviewing (MI) to come alongside Marci by using a client-centered approach to encouraging abstaining from harmful drinking and smoking (Miller & Rollnick, 2013).
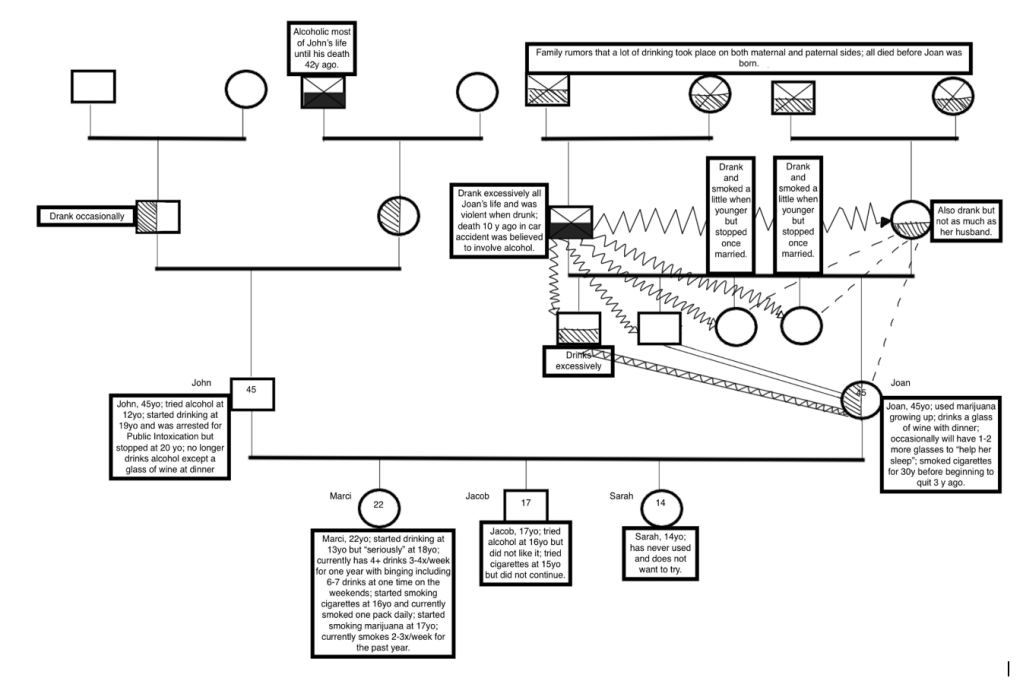
- Review of the family genogram. Reviewing this genogram has the potential to open Marci’s eyes to the issues being passed down throughout her family, especially along with learning about the 50-60% of heritability of Alcohol Use Disorders and its ties to anxiety (Pandey et al., 2017).
- Use of smartphone apps that aid in learning about blood alcohol concentration as well as skill-training to avoid drinking (Gajecki et al., 2017).
Several resources are available for the client. However, because Marci has repeatedly not shown a desire for change, it would be wise to wait until she moves towards the next stage in the change process before suggesting.
- Based on Marci’s genetic predisposition to alcoholism, a resource which educates her on the risks of abusing alcohol would be useful. Based on her age group, the apps previously mentioned might be a best resource.
Questions
There are several questions I would have wanted to ask that did not get asked or shown. As it pertains to the AUDIT Interview, I would have also wanted to know the following:
- Was there ever a time when you felt you could not stop drinking once you had started?
- Have you ever felt like you needed a drink first thing in the morning after a heavy drinking session?
- Have you ever been unable to remember what happened the night before because you had been drinking?
After reviewing the narrative presented, I also had the following questions:
- What was your reason to abstain from smoking cigarettes six months ago?
- Is there any event you can remember that came shortly before your feelings of sadness and too much worry started increasing?
- What form of birth control do you use?
- Can you tell me more about your desire to become an attorney?
- When was the last time you had a full physical medical exam?
- How would you like your relationship with your parents to look?
- How would you describe your relationship with Yahuah?
- What expectations do you have for yourself?
Diagnostic Impressions
All of the following diagnostic impressions, prevalence, culture/gender issues, functional consequences, comorbidity, and possible differential diagnosis listed are taken from the Diagnostic and statistical manual of mental disorders (5th ed.; DSM-5; American Psychiatric Association, 2013) unless stated otherwise. Supporting statements for listed criteria come from Liberty University’s addictions case study narrative on “Marci”.
Primary Diagnostic Impression
Primary Diagnosis – Listing of Criteria Met
F10.20 Alcohol Use Disorder, Severe
- A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or recover from its effects.
- Recreational and social interests had increasingly involved the use of alcohol.
- Craving, or a strong desire or urge to use alcohol.
- Marci had been drinking four or more alcoholic beverages three to four times a week for one year. She would also go on weekend binges starting to drink Friday evenings, have a glass or two of wine around lunchtime on Saturday, having six to seven beers Saturday evenings, and one to two glasses of wine when alone on school nights.
- Recurrent alcohol use resulting in a failure to fulfill major role obligations at work, school, or home.
- On the mornings after she used alcohol, Marci tended to sleep in and cut class, but not every week.
- Over the past four years, she has been fired or left three other places of employment due to excessive absenteeism and once for destruction of property.
- Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused by or exacerbated by the effects of alcohol.
- Since her arrest, her recreational and social interests are still involving the use of alcohol.
- After her DUI, her parents sat her down and expressed their concern about the amount she was drinking and want her to stop. Since their confrontation and her arrest, she did cut down somewhat on her use of both alcohol and marijuana, and (when pressed by her parents) she would abstain for several weeks at a time.
- Recurrent alcohol use in situations in which it is physically hazardous.
- Marci was arrested five months ago for driving while impaired with a blood alcohol level of 0.13. Her license was suspended, but she has driving privileges to get to school/work and back.
- Alcohol use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by alcohol.
- Over the past three years she has had two accidents that occurred while she was intoxicated with alcohol and marijuana, but no other people or vehicles were involved, and no charges were filed against her.
- Her use of alcohol has not changed since she was arrested.
Prevalence, Culture/Gender Issues, Functional Consequences, Comorbidity
Prevalence rates of alcohol use disorder reveal it to be common in the population. It is most common in 18- to 29-years-old, with an estimated 16.2% of individuals in this range. Men are more likely to experience this disorder than women, at rates of 12.4% and 4.9%, respectively.
Across most cultures, alcohol is often the most commonly used intoxicating substance. About 80% of adults, ages 18 and over, have reported consuming alcohol at some point in their lives. Additionally, 65% have reported drinking within the past year, and can therefore be called current drinkers. Out of the 3.6% of the population in the world which classify for alcohol use disorder, 5.2% are found in the Americas.
Gender differences arise in that women – due to normally being lower in weight, having more fat and less water in the body, and metabolizing lower amounts of alcohol – are increasingly likely to have a higher blood alcohol concentration per drink than men. Women who often consume large quantities of alcohol are also more likely to develop physical consequences. Nevertheless, the rate of drinking disorders among men is higher than women.
Functional consequences of alcohol use disorder may include the disruption of some major areas of functioning in everyday life, such as school, work, driving, relationships, and health. The risk of driving and violence is increased with this disorder. Alcohol accounts for 55% of fatalities in driving accidents. Additionally, the use of alcohol in this disorder can lead to feelings of sadness and irritability, which could possibly lead to suicide attempts and completions.
Comorbidity may include disorders such as anxiety and depression. Physical manifestations due to reduced immunological function may also lead to increased possibility of infections and risk of cancers.
Possible Differential Diagnoses
A possible differential diagnosis going forward is nonpathological use of alcohol depending on the decisions she makes going forward.
Secondary Diagnostic Impressions
Secondary Diagnosis 1 – Listing of Criteria Met
F12.20 Cannabis Use Disorder, Moderate
- Craving, or a strong desire or urge to use cannabis.
- Marci had been smoking marijuana two to three times a week for one year. She would also go on weekend binges smoking Friday evenings, smoking 1-2 joints around lunchtime on Saturday, 1-2 joints Saturday afternoons, several joints Saturday evenings, and half a joint when alone on school nights.
- She says that she finds marijuana pleasurable and relaxing and that, if she could find a way to not get caught, she would like to continue using it.
- Recurrent cannabis use resulting in a failure to fulfill major role obligations at work, school, or home.
- When her parents first discovered her marijuana use, they insisted that she seek professional help for what they perceived to be a drug problem. Although they even threatened to call her college academic dean because of her dropping grades, Marci refused help and began to discuss quitting school.
- Important social, occupational, or recreational activities are given up or reduced because of cannabis use.
- Recreational and social interests had increasingly involved the use of marijuana.
- Marci admits that, since she began smoking marijuana, her previously good and trusting relationship with her parents has soured. She had begun to hide and lied to them about using, and had felt increasingly negative about herself, especially as her grades have suffered and her general interests have narrowed.
- It was not until her arrest that she began to feel some guilt and remorse over the fact that her drinking and especially her marijuana use was negatively impacting her relationship with her parents, and interfering with her desire to be an attorney.
- She had also become gradually aware that marijuana had been affecting her motivation, her schoolwork, and her spiritual life.
- Recurrent cannabis use in situations in which it is physically hazardous.
- Marci was charged with possession of a small amount (about 1 gram) of marijuana when she was arrested for driving while intoxicated.
Prevalence, Culture/Gender Issues, Functional Consequences, Comorbidity
Cannabis is one of the most used psychoactive illicit drugs in the United States. Cannabis use disorder is found in higher rates among males than females, with the highest rate of use being in the age range of 18- to 29-year-olds. A higher prevalence rate of cannabis use disorder is found among 12- to 17-year-olds (3.4%) than among adults 18 years and over (1.5%); this is thought to be due to the wide availability of this drug in the United States.
Moderate cultural differences exist among prevalence rates with Native American and Alaska Natives having the highest rate of cannabis use disorder among both the younger age group and the adult group. Males are more likely to experience cannabis use disorder among the adult group, with a smaller difference in the younger group, although still more likely.
Functional consequences of cannabis use disorder include impairment of higher executive function, which can cause issues at school or work. There could also be problems related to social relationships. Completing tasks, such as driving or working under the influence, can lead to accidents. Due to the carcinogenic compounds in cannabis smoke, respiratory illnesses are possible. Additionally, mental disorders can be brought on or made worse through chronic cannabis use.
Comorbidity with other substance use disorders and mental conditions is common. More than half of those with cannabis use disorder also have alcohol use disorder and tobacco use disorder. Mental conditions common among those with cannabis use disorder include major depressive disorder, anxiety disorder, and bipolar I disorder.
Possible Differential Diagnoses
It is important to attempt to differentiate between the effects of other co-occurring diagnosis with cannabis use disorder. Some of the consequences may be due to alcohol use disorder rather than cannabis use disorder. Therefore, a differential diagnosis of nonproblematic use of cannabis can be explored. It is also important to consider other mental disorders as a differential diagnosis based on reported levels of sadness and worry.
Secondary Diagnosis 2 – Listing of Criteria Met
Z72.0 Tobacco Use Disorder, Mild
- There is a persistent desire or unsuccessful efforts to cut down or control tobacco use.
- She has smoked cigarettes since age 16 and currently smokes one pack daily. Marci stopped smoking cigarettes for six months one year ago, but she presently does not plan to cut down or quit.
- Tobacco use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by tobacco.
- She says every now and then, especially during allergy season, she tends to get a “dry, hacky cough.”
Prevalence, Culture/Gender Issues, Functional Consequences, Comorbidity
Tobacco/nicotine is mostly consumed as cigarettes. 21% of adults in the United States are current smokers and approximately 80% of those are daily smokers. Males and females have a similar prevalence rate.
Culturally, Native American and Alaska Natives have the greatest prevalence rates. Non-Hispanic white smokers seem to be more likely to develop tobacco use disorder. Some ethnic differences might be based on biology, affecting nicotine blood levels and nicotine metabolism speed.
Functional consequences of tobacco use disorder tend to develop over time and often begin when they reach their 40s. Half of smokers who choose to continue smoking die prematurely from an illness related to tobacco. Most conditions develop from exposure to other components of tobacco besides nicotine.
Comorbidity with medical issues such as perinatal problems, miscarriage, cardiovascular illnesses, cancers, and pulmonary disease are common. There is also comorbidities with disorders such as alcohol and substance use disorders, depression, anxiety.
Possible Differential Diagnoses
There are no differential diagnosis present.
F32.9 Unspecified Depressive Disorder
- The following symptoms have been present during the same 2-week period and represent a change from previous functioning (5th ed.; DSM-5; American Psychiatric Association [APA], 2013).
- Depressed mood for most of the day, nearly every day, as indicated by subjective report (APA, 2013) [feelings of sadness and worrying too much about two months ago].
- Markedly diminished interest or pleasure in almost all activities of the day, nearly every day (APA, 2013) [On the mornings after she used alcohol, Marci tended to sleep in and cut class, but not every week. Her recreational and social interests had increasingly involved the use of alcohol and marijuana, now since her arrest, it is mainly alcohol (although she still desires to smoke cannabis)].
Prevalence, Culture/Gender Issues, Functional Consequences, Comorbidity
Prevalence rates indicate up to three times higher percentages among the ages of 18- to 29-years old and women (APA, 2013). Culturally, there are many differences in prevalence rates, except for the consistency of the female-to-male ratio (APA, 2013). The most common symptoms reported are insomnia and loss of energy (APA, 2013). Prevalence among women is a chief gender issue, however, when it comes to symptoms, consequences, and treatments there are no clear differences among the genders (APA, 2013). Functional consequences include a wide margin of impairment (APA, 2013). Often there will be physical symptoms reported, as well as reports of decreased functioning in most areas of life (APA, 2013). With regards to comorbidity, major depressive disorder tends to occur along with substance-related disorders, panic disorders, obsessive-compulsive disorders, anorexia and bulimia nervosa, and borderline personality disorder (APA, 2013).
Possible Differential Diagnosis
Possible differential diagnosis for Marci include mood disorder due to another medical condition, substance/medication-induced depressive disorder, and sadness (APA, 2013).
F41.9 Unspecified Anxiety Disorder
- The individual finds it difficult to control the worry (APA, 2013) [Marci has begun to express concern to her friends about “feeling depressed and anxious,”].
- The anxiety and worry are associated with sleep disturbance (APA, 2013) [she has only a few problems regarding sleeping (trouble sleeping soundly, getting up too late)].
Prevalence, Culture/Gender Issues, Functional Consequences, Comorbidity
Prevalence rates indicate that about 2.9% of adults develop generalized anxiety disorder (APA, 2013). Culturally, it is important to consider the social and cultural context in determining whether worries are excessive (APA, 2013). It has also been found that European descent may be a factor in experiencing generalized anxiety disorder (APA, 2013). Gender issues reflect a double risk for women when compared to men in experiencing generalized anxiety disorder, especially comorbid with unipolar depression (APA, 2013). Functional consequences include the impairment of being able to complete tasks quickly and efficiently and can lead to disability (APA, 2013). The main comorbidity patterns include depressive disorders and substance use disorders, especially in men (APA, 2013).
Possible Differential Diagnosis
Possible differential diagnosis include substance/medication-induced anxiety disorder and depressive disorders (APA, 2013).
Treatment Plan
Treatment Plan Problem/Symptom 1
Client exhibits symptoms of alcohol use disorder manifested by increased recreational and social interests involving the use of alcohol; craving or strong desire to use alcohol; failure to fulfill major role obligations at work, school, and home; continued alcohol use despite having recurrent problems caused by the effects of alcohol; recurrent alcohol use in situations in which it is physically hazardous; and continued alcohol use despite knowledge of having a recurrent physical and psychological problem likely to have been caused by alcohol (5th ed.; DSM-5; American Psychiatric Association [APA], 2013).
Long-Term Goal 1
Client will accept the powerlessness and unmanageability over mood-altering substances and participate in a recovery-based program (Perkinson et al., 2014). Participating in a 12-step program will increase the likely hood of treatment being successful since they have been shown to complement and extend the effects of professional treatment (National Institute on Drug Abuse [NIDA], 2018).
Short-Term Goal/Objective 1
Client will attend Alcoholics Anonymous meetings as frequently as necessary to support sobriety (Perkinson et al., 2014). This will be measured by reporting on the impact of the meetings and processing of messages the client is receiving (Perkinson et al., 2014).
Short-Term Goal/Objective 2
Client will learn about the Alcoholics Anonymous concept of a higher power and how this can assist in recovery. This will be measured by completing an Alcoholics Anonymous Step 1 paper and presenting it to therapist, completing Step 2 and Step 3 exercises from The Alcoholism & Drug Abuse Patient Workbook by Perkinson (Perkinson et al., 2014).
Long-Term Goal 2
Client will resolve ambivalence and utilize behavioral and cognitive coping skills to help maintain sobriety (Perkinson et al., 2014). Cognitive behavioral therapy (CBT) has been shown to be an effective evidence-based therapy for individuals with skills learned during therapy remaining after completion of treatment (NIDA, 2018).
Short-Term Goal/Objective 1
Client will explore and resolve ambivalence associated with commitment to change behaviors related to substance use and addiction (Perkinson et al., 2014). This will be measured by conducting Motivational Interviewing (Miller & Rollnick, 2013) and making a list of ways substance use has affected her life (Perkinson et al., 2014).
Short-Term Goal/Objective 2
Client will identify, challenge, and replace destructive, high-risk self-talk with positive, strength-building self-talk (Perkinson et al., 2014). This will be measured by rehearsing situations in which the client identifies her negative self-talk and generates empowering alternatives (Perkinson et al., 2014).
Treatment Plan Problem/Symptom 2
Client exhibits symptoms of cannabis use disorder in remission manifested by a strong desire to use cannabis; recurrent use resulted in a failure to fulfill major role obligations at work, school, or home; important occupational and recreational activities were reduced due to cannabis use; and recurrent cannabis use in situations in which it was physically hazardous (APA, 2013).
Long-Term Goal 1
Client will establish a sustained recovery, free from the use of all mood-altering substances (Perkinson et al., 2014). Sustained abstinence can be hindered by several triggers, yet research demonstrates that active participation in treatment is conducive to good outcomes (NIDA, 2018).
Short-Term Goal/Objective 1
Client will verbalize increased knowledge of substance use and the process of recovery (Perkinson et al., 2014). This will be measured by assigning reading of a workbook describing evidence-based treatment approaches to addiction recovery and using the readings to reinforce key concepts and practices throughout therapy (Perkinson et al., 2014).
Short-Term Goal/Objective 2
Client will verbalize an understanding of factors that can contribute to development of chemical dependence and pose risks for relapse (Perkinson et al., 2014). This will be measured by assessing understanding of her genetic, personality, social, and family factors that led to the development of chemical dependency and serve as risk factors for relapse (Perkinson et al., 2014).
Long-Term Goal 2
Client will establish and maintain total abstinence, while increasing knowledge of the disease and the process of recovery (Perkinson et al., 2014). Increasing knowledge can be achieved through a collaborative and positive therapeutic relationship (NIDA, 2018).
Short-Term Goal/Objective 1
Client will learn and implement communication and problem-solving skills toward achieving goals within the therapeutic relationship (Perkinson et al., 2014). This will be measured by using modeling, role-playing, and behavioral rehearsal (Perkinson et al., 2014).
Short-Term Goal/Objective 2
Client will verbalize an understanding of lapse and relapse (Perkinson et al., 2014). This will be measured by evaluating past lapses and utilizing self-monitoring to assess current risks (Perkinson et al., 2014).
Treatment Plan Problem/Symptom 3
Client exhibits symptoms of unspecified depressive disorder manifested by feelings of sadness increasing in the past two months and diminished interest or pleasure in almost all activities (APA, 2013).
Long-Term Goal 1
Client will elevate mood and develop a program of recovery free from addiction (Perkinson et al., 2014). According to Moos (2003), the most effective models of treatment for clients with dual diagnosis are those that integrate psychiatric care with substance abuse, therefore an approach which addresses her depression in light of her addiction would be the most effective.
Short-Term Goal/Objective 1
Client will identify a pattern of using drug or alcohol abuse as a means of escaping from depression and verbalize more constructive means of coping (Perkinson et al., 2014). This will be measured by evidence of client processing healthier, more constructive means of coping with depression such as sharing pain with others, attending 12-step recovery program meetings, developing positive cognitions, taking medication, turning conflicts over to a higher power, practicing gratitude (Perkinson et al., 2014).
Short-Term Goal/Objective 2
Client will write an aftercare program (Perkinson et al., 2014). This will be measured by the development of a written aftercare program that includes regular attendance at 12-step recovery groups and any other therapy that the client needs to improve her health (Perkinson et al., 2014).
Long-Term Goal 2
Client will develop healthy thinking patterns and beliefs about self, others, and the world that lead to the alleviation and help prevent the relapse of depression (Perkinson et al., 2014). A meta-analysis of long-term effects of CBT treatment for depression reported lower relapse rates after follow-ups 1 and 2 years later than pharmacotherapy alone (Cuijpers et al., 2013).
Short-Term Goal/Objective 1
Client will identify and replace thoughts and beliefs that support depression (Perkinson et al., 2014). This will be measured by assigning self-monitoring of thoughts, feelings, and actions in a daily journal while CBT is being conducted (Perkinson et al., 2014).
Short-Term Goal/Objective 2
Client will learn and implement behavioral strategies to overcome depression (Perkinson et al., 2014). This will be measured by assessing skills developed that increase likelihood of deriving pleasure from behavioral activation (Perkinson et al., 2014).
Treatment Plan Problem/Symptom 4
Client exhibits symptoms of unspecified anxiety disorder manifested by increased feelings of worry in the past two months; finding it difficult to control the worry; and the anxiety and worry are associated with sleep disturbance (APA, 2013).
Long-Term Goal 1
Client will end addiction as a means of escaping anxiety and practice constructive coping behaviors (Perkinson et al., 2014). The withdrawal stage of substance use can result in emotional symptoms such as anxiety based on a reduced activation in the reward systems of the brain and an increase in the activation of the stress systems of the brain, leading to using the substance in order to alleviate the symptoms (National Institute on Alcohol Abuse and Alcoholism [NIAAA], 2021).
Short-Term Goal/Objective 1
Client will acknowledge the powerlessness and unmanageability caused by excessive anxiety and addiction (Perkinson et al., 2014). This will be measured by understanding of the relationship between anxiety and addiction (Perkinson et al., 2014).
Short-Term Goal/Objective 2
Client will verbalize an understanding of the cognitive, physiological, and behavioral components of anxiety and its treatment (Perkinson et al., 2014). This will be measured by reading psychoeducational sections of books or treatment manuals on worry and generalized anxiety (Perkinson et al., 2014).
Long-Term Goal 2
Client will learn and implement coping skills that result in a reduction of anxiety and worry, and improved daily functioning (Perkinson et al., 2014). Learning coping skills helps reduce anxiety because “fear and anxiety are defused by knowledge” (Clinton & Langberg, 2011, p.142).
Short-Term Goal/Objective 1
Client will learn and implement calming skills to reduce overall anxiety and manage anxiety symptoms (Perkinson et al., 2014). This will be measured by the application of skills in her daily life (Perkinson et al., 2014).
Short-Term Goal/Objective 2
Client will learn and implement a strategy to limit the association between various environmental settings and worry, delaying the worry until a designated “worry time” (Perkinson et al., 2014). This will be measured by the implementation of a worry time (Perkinson et al., 2014).
References
Gajecki, M., Andersson, C., Rosendahl, I., Sinadinovic, K., Fredriksson, M., & Berman, A. H.
(2017). Skills training via smartphone app for university students with excessive alcohol consumption: A randomized controlled trial. International Journal of Behavioral Medicine, 24(5), 778–788. https://doi.org/10.1007/s12529-016-9629-9
Hart, C.L. & Ksir, C.J. (2018). Drugs, society, & human behavior (17th ed.). McGraw-Hill
Education.
Miller, W. R., & Rollnick, S. (2013). Motivational interviewing: Helping people change (3rd ed.).
The Guilford Press.
Pandey, S.C., Kyzar, E.J., Zhang, H. (2017). Epigenetic basis of the dark side of alcohol
addiction. Neuropharmacology, 122, 74-84. https://doi.org/10.1016/j.neuropharm.2017.02.002
The Scriptures. (2018). Institute for Scripture Research.
The Stages of Change (n.d.). The stages of change [PDF]. Liberty University.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders
(5th ed.).
Clinton, T. & Langberg, D. (2011). The quick-reference guide to counseling women. Baker
Books.
Cuijpers, P., Berking, M., Andersson, G., Quigley, L.,M., Kleiboer, A., & Dobson, K. S. (2013).
A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Canadian Journal of Psychiatry, 58(7), 376-85. http://ezproxy.liberty.edu/login?qurl=https%3A%2F%2Fwww.proquest.com%2Fscholarly-journals%2Fmeta-analysis-cognitive-behavioural-therapy-adult%2Fdocview%2F1426313762%2Fse-2
Miller, W. R., & Rollnick, S. (2013). Motivational interviewing: Helping people change (3rd ed.).
The Guilford Press.
Moos, R.H. (2003). Addictive disorders in context: Principles and puzzles of effective treatment
and recovery. Psychology of Addicted Behaviors, 17(1), 3-12.
National Institute on Alcohol Abuse and Alcoholism. (2021). The cycle of alcohol addiction.
National Institute of Health.
National Institute on Drug Abuse. (2018). Principles on drug addiction treatment: A research
based guide (3rd ed.). National Institute of Health.
Perkinson, R. R., Jongsma, A.E., & Bruce, T.J. (2014). The addiction treatment planner (5th ed.).
John Wiley & Sons, Inc.
